
Addressing inflammatory back pain (IBP) necessitates prescription medication, typically a nonsteroidal anti-inflammatory medicine (NSAID).
The good news is that you should be able to control the pain brought on by IBP if you follow the treatment plan suggested by your doctor.
Adherence to medical therapy is critically important. With currently available treatments, progression can be stopped, but non-adherence can result in loss of efficacy and, ultimately, progression. Serious consequences, such as spinal abnormalities and fractures, might result from progression. Furthermore, if your symptoms are worsened, you may be unable to work or engage in your typical daily activities.
However, there are a number of actions you may do to manage your inflammatory back pain in addition to adhering to the course of therapy advised by your physician:
1. Exercise regularly to reduce inflammatory back pain
In contrast to mechanical back pain [1], which can become worse with exercise, inflammatory back pain (IBP) often gets better after engaging in the appropriate physical activity. Your doctor should advise you to visit a physical therapist so you may learn stretches and exercises that can ease your back discomfort and strengthen the muscles surrounding it.
Stretches can also be beneficial. Programs such as the The Miracle Back Pain and My Back Pain Coach provide stretching techniques and exercises to improve back pain.
While dealing with inflammatory back pain, it is generally recommended to stay physically active and perform muscle strengthening and stretching activities. But because they could damage your spine, you should avoid activities with excessive impact.
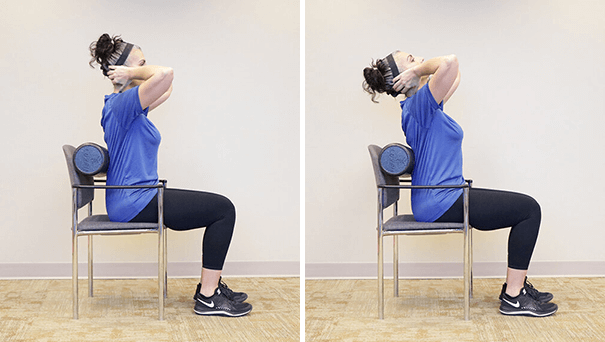
The sitting thoracic extension is a helpful stretch for IBP. Put your feet level on the floor and your back straight on the chair’s back as you sit in a low-back chair to perform this stretch. Then, with your elbows extended, rest your hands behind your head (or, if it’s more comfortable for you, cross your arms over your chest). Slowly lean backward until the top of your spine touches the chair’s back while keeping your head motionless. Return to your starting position after holding this posture for ten seconds.
2. Learn how to properly lift heavy items
Simple breathing exercises often entail repeatedly taking deep breaths in and out to both increase lung capacity and decrease any inflammation in the joints that link the ribs to the spine (the rib joints).
Your rib joints may be impacted if IBP develops into ankylosing spondylitis, which it frequently does. This could restrict how much your rib cage can move up and down when you breathe, making it more difficult for your lungs to function normally, especially when engaging in heavy activity.
3. Select the ideal mattress
The appropriate mattress won’t treat your IBP, but it might make it easier for you to sleep with good posture.
A firm mattress that is not too hard and not too soft is recommended.
In order to help maintain excellent posture, he also advises persons with inflammatory back pain to try sleeping on their abdomen for about 30 minutes each night.
You may feel better overall if you get enough sleep. In a study published in July 2019 in the Scandinavian Journal of Pain [2], poor sleep was associated with persistent low back pain [3].
4. Engage in deep breathing exercises to keep your lungs healthy
Simple breathing exercises often entail repeatedly taking deep breaths in and out to both increase lung capacity and decrease any inflammation in the joints that link the ribs to the spine (the rib joints).
Your rib joints may be impacted if IBP develops into ankylosing spondylitis, which it frequently does. This could restrict how much your rib cage can move up and down when you breathe, making it more difficult for your lungs to function normally, especially when engaging in heavy activity.
5. Make your home fall-proof to prevent fractures
It’s important to make your home safe in order to reduce the risk of falling and slipping. Noting that inflammatory back pain raises the likelihood of spinal fractures, hence the importance of avoiding falls.
Avoid having “trip sites” in your home, such as crowded areas or corners with rolled-up rugs, and use caution when climbing stairs and entering and exiting the shower or bathtub. In the kitchen and bathroom, non-slip rugs or floor mats might also be useful.
6. Make your workspace posture-friendly.
Look for measures to enhance your posture at work if you have inflammatory back pain and are working because the issue often develops around the age of 40. Think about using a standing desk, or request an ergonomic chair from your work, or perhaps use both. Instead of only practicing one or the other, you could discover that switching between standing and sitting is more beneficial.
You can lessen the pressure on your spine by placing your phone or computer screen and keyboard so that you are not slumped over your desk while working or compelled to reach across your desk to get stuff. Sitting on chairs with good low-back support and in a straight, upright stance is very important. Additionally, if you spend a lot of time sitting at your desk at work, you should get up often to stretch and maintain flexibility. Avoid sitting down for extended periods of time; ideally, limit it to no more than 30 minutes at a time [4].
7. For back comfort, consider a raised toilet seat
Conclusion
Among the tips that we presented in this article, number one tip is to stay active to prevent/improve your back pain. We highly suggest reading our article Top Back Pain Causes and How to Alleviate Your Back Pain to learn more about the common causes of back pain.
Supporting Sources
[1] Inflammatory vs. Mechanical Back Pain. Spondylitis Association of America. https://spondylitis.org/About-Spondylitis/Inflammatory-vs-Mechanical-Back-Pain/
[2] Vanti C, Andreatta S, Borghi S, Guccione AA, Pillastrini P, Bertozzi L. The effectiveness of walking versus exercise on pain and function in chronic low back pain: a systematic review and meta-analysis of randomized trials. Disabil Rehabil. 2019 Mar;41(6):622-632. doi: 10.1080/09638288.2017.1410730. Epub 2017 Dec 5. PMID: 29207885.
[3] Vinstrup J, Jakobsen MD, Andersen LL. Poor Sleep Is a Risk Factor for Low-Back Pain among Healthcare Workers: Prospective Cohort Study. Int J Environ Res Public Health. 2020 Feb 5;17(3):996. doi: 10.3390/ijerph17030996. PMID: 32033339; PMCID: PMC7036951.
[4] Rodríguez-Romero B, Smith MD, Pértega-Díaz S, Quintela-Del-Rio A, Johnston V. Thirty Minutes Identified as the Threshold for Development of Pain in Low Back and Feet Regions, and Predictors of Intensity of Pain during 1-h Laboratory-Based Standing in Office Workers. Int J Environ Res Public Health. 2022 Feb 16;19(4):2221. doi: 10.3390/ijerph19042221. PMID: 35206409; PMCID: PMC8871560.
This article does not provide medical advice. It is intended for informational purposes only. It is not a substitute for professional medical advice, diagnosis or treatment. Never ignore professional medical advice in seeking treatment because of something you have read on the healthysolutions.fit Site. If you think you may have a medical emergency, immediately call your doctor or dial 911.
Related Articles

